
Thus, an expansion of alveolar macrophage pool sizes may be observed in both septic ARDS patients and in experimental animal models with ARDS-like inflammatory phenotypes, and expanded alveolar macrophage pools may be involved in remote lung injury developing in response to systemic inflammation.
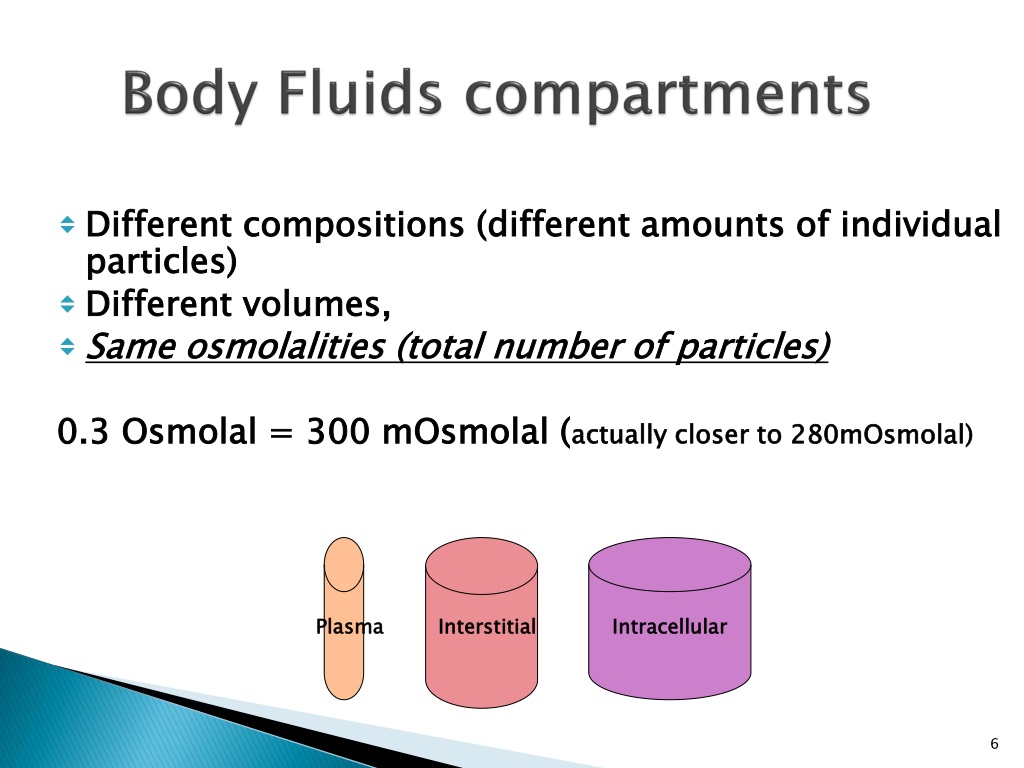
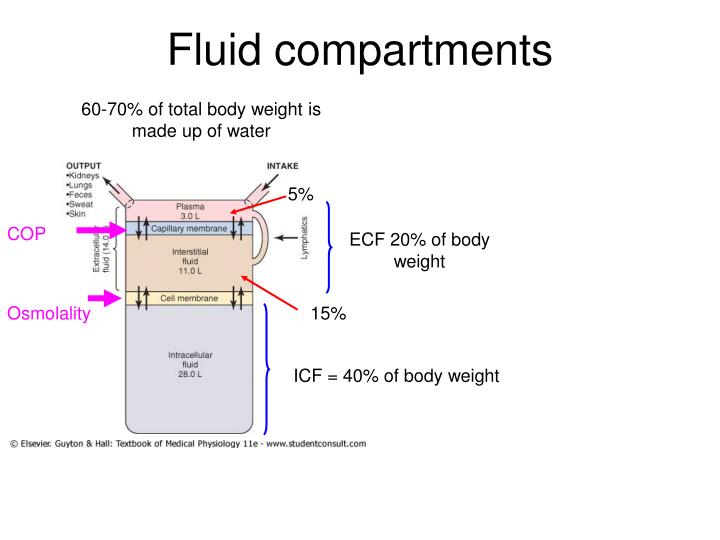
Body fluid compartments dunnet plus#
In addition, we recently showed in an animal model that intratracheal application of CCL2 plus LPS synergistically induced acute lung inflammation, indicating that monocytes that are recruited into the lungs of mice may both expand the alveolar macrophage pool and aggravate LPS-induced neutrophilic alveolitis and lung injury in mice. We have recently demonstrated alveolar accumulations of CD14-positive mononuclear phagocytes and elevated BAL fluid CCL2 levels together with an expanded alveolar macrophage pool correlating with increased lung injury scores in patients with sepsis related ARDS. Clearly, both newly recruited alveolar monocytes and resident macrophages are potentially involved in the overall lung inflammatory response. Previously published studies employing a two hit model of initial intraperitoneal LPS challenge to trigger sepsis-induced remote lung inflammatory responses followed by a secondary intratracheal LPS challenge to mimic the additional development of pneumonia have not addressed changes in alveolar macrophage pool sizes and related functional consequences. In particular, it is unclear whether such expanded alveolar macrophage pools in septic ARDS patients are functionally relevant in terms of aggravating lung inflammatory responses to secondary pneumonia, which complicate the later phase of septic ARDS. Īlthough expansion of alveolar macrophage populations in septic ARDS patients is a well described phenomenon, the underlying molecular events shaping this leukocytic response are not known. Key chemokines involved in this process of lung leukocyte invasion include the main monocyte chemoattractant CCL2 and the neutrophil chemoattractants MIP-2, KC and MIP-1α. In human studies, patients who develop ARDS have highly elevated serum and alveolar cytokine and chemokine levels that are associated with a massive accumulation of neutrophils within the lungs, expanded alveolar macrophage populations and increased lung injury scores. For example, experimental animal models of endotoxin (lipopolysaccharide, LPS) induced acute peritonitis have characterized the kinetics of intraperitoneal LPS resorption and its rapid appearance within the vascular compartment within minutes to hours. The molecular events eliciting sepsis-related complications such as acute lung injury have only been partially defined. Acute respiratory distress syndrome (ARDS) and multiorgan failure are frequent complications of severe sepsis that contribute to the morbidity and mortality of this critical illness. Overwhelming innate immune responses to systemic inflammation contribute to the clinical manifestation of sepsis and septic shock. This finding represents a previously unrecognized novel inflammatory component of lung inflammation that results from endotoxin-induced peritonitis. These data, taken together, show that intraperitoneal endotoxin triggers a CCR2-dependent de novo recruitment of monocytes into the lungs of mice but this does not result in an accentuation of neutrophilic lung inflammation. An intentional two-fold expansion of alveolar macrophage numbers by intratracheal CCL2 following intraperitoneal endotoxin did not exacerbate the development of acute lung inflammation in response to intratracheal endotoxin compared to mice challenged only with intratracheal endotoxin. In contrast, expansion of the alveolar macrophage pool was not observed in CCR2-deficient mice and in wild-type mice systemically pretreated with the anti-CD18 antibody GAME-46. We observed that mice challenged with intraperitoneal endotoxin developed rapidly increasing serum and bronchoalveolar lavage fluid (BALF) cytokine and chemokine levels (TNFα, MIP-2, CCL2) and a nearly two-fold expansion of the alveolar macrophage population by 96 h, but this was not associated with the development of neutrophilic alveolitis.
Serum and lavage cytokines as well as bronchoalveolar lavage fluid cells were analyzed at different time points after intraperitoneal or intratracheal application of LPS.
We hypothesized that endotoxin-induced peritonitis provokes recruitment of monocytes into the lungs, which amplifies lung inflammatory responses to a second hit intra-alveolar challenge with endotoxin. Acute peritonitis developing in response to gram-negative bacterial infection is known to act as a trigger for the development of acute lung injury which is often complicated by the development of nosocomial pneumonia.


 0 kommentar(er)
0 kommentar(er)
